News
Behind the Headlines
Two-Cents Worth
Video of the Week
News Blurbs
Articles
Testimony
Bible Questions
Internet Articles (2015)
Internet Articles (2014)
Internet
Articles (2013)
Internet Articles (2012)
Internet Articles (2011)
Internet Articles (2010)
Internet Articles
(2009)
Internet Articles (2008)
Internet Articles (2007)
Internet Articles (2006)
Internet Articles (2005)
Internet Articles (2004)
Internet Articles (2003)
Internet Articles (2002)
Internet Articles (2001)


 y
heart attack was caused by blockages in three major arteries—two
on the top of my heart and one on the bottom. Three out of 12 chances
to have a major heart attack. But, when it comes to blockages that cause
fatal heart attacks, men have it easy. Easier, that is, than women. Unless
we have three or more arteries or coronary veins that are blocked 90%
to 100%, you might say we have only a 1-in-12 chance of dying from our
first heart attack. High-risk women have a 1-in-2, or 50% chance of their
first heart attack killing them. Men—even the stupid ones like me
that ignored the symptoms for over a year and even refused to go to the
hospital when I had a significant heart attack on Christmas Eve, 2000—generally
survive a first heart attack.
y
heart attack was caused by blockages in three major arteries—two
on the top of my heart and one on the bottom. Three out of 12 chances
to have a major heart attack. But, when it comes to blockages that cause
fatal heart attacks, men have it easy. Easier, that is, than women. Unless
we have three or more arteries or coronary veins that are blocked 90%
to 100%, you might say we have only a 1-in-12 chance of dying from our
first heart attack. High-risk women have a 1-in-2, or 50% chance of their
first heart attack killing them. Men—even the stupid ones like me
that ignored the symptoms for over a year and even refused to go to the
hospital when I had a significant heart attack on Christmas Eve, 2000—generally
survive a first heart attack.
The classic symptoms everyone
with an ounce of common sense recognizes as signs that you're having a
heart attack had been prevalent for well over a year—stabbing pain
in the lower jaw, gripping pain in the chest, and an almost ritualistic
numbing sensation in my left arm—every morning as I rushed through
Union Station in Washington, DC to catch the Washington Times shuttle
for the fifteen minute ride to my office. An ardent believer in the power
of prayer to heal, I prayed healing over my body every time my body warned
me it was past time to see a cardiologist, confident that the Master Physician
would clear the blockages and heal my body. 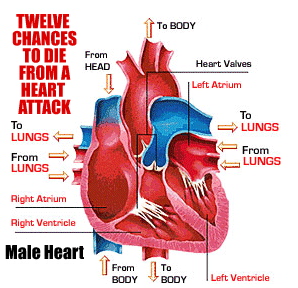 When
I finally ran out of warnings and had my heart attack I had ignored some
very serious symptoms for at least six months. Simple, routine tests performed
at my local hospital or doctor's office would have confirmed what I already
knew to be true. Very likely, immediate treatment would have prevented
the triple bypass I had in July, 2001. Had I gone to the doctor early
enough, an angioplasty would have prevented the heart attack that ultimately
required a 3 1/2 hour triple bypass to repair.
When
I finally ran out of warnings and had my heart attack I had ignored some
very serious symptoms for at least six months. Simple, routine tests performed
at my local hospital or doctor's office would have confirmed what I already
knew to be true. Very likely, immediate treatment would have prevented
the triple bypass I had in July, 2001. Had I gone to the doctor early
enough, an angioplasty would have prevented the heart attack that ultimately
required a 3 1/2 hour triple bypass to repair.
Generally speaking, its not
that easy for women. Doctors have known ever since the pathologists began
mapping the anatomical and physiologically distinctions between the sexes
that men and women are at different mortality risks—even with the
same illnesses and diseases. It is generally much easier to detect coronary
disease in men than in women since in men, it is usually the larger, easier-to-detect
coronary arteries that get blocked. With women, more commonly, heart disease
begins when plaque builds in the smallest heart arteries, ever so slowly
reducing the oxygen flow to the larger arteries that seldom become clogged,
making it much more difficult for physicians to correctly diagnose female
heart disease. Standard chest X-rays, catscans and angiographies usually
miss the problem, and pulmonary problems usually become the suspect of
choice. What
brings the woman to her family physician is not the warning signs that
suggest heart disease, but signs that suggest she is simply overworked
since fatigue, a lack of energy and shortness of breath are the most common
symptoms. Or, she may experience flu-like symptoms, complete with nausea,
clamminess and cold sweat. Or, she may simply feel apprehensive and discomforted
with a loss of appetite. Less than one in three women who suffer a heart
attack feel chest pain or pain in the upper back, shoulders, neck, jaw
or left arm. 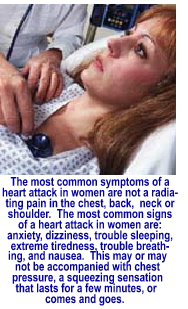 Many
times, heart symptoms for women are mistaken for neuroticism or depression—particularly
when an angiography shows nothing abnormal. Where approximately 63% of
the women who die from sudden-death heart attacks have coronary microvascular
syndrome [CMS], less than 20% of men do.
Many
times, heart symptoms for women are mistaken for neuroticism or depression—particularly
when an angiography shows nothing abnormal. Where approximately 63% of
the women who die from sudden-death heart attacks have coronary microvascular
syndrome [CMS], less than 20% of men do.
And, for those of us males who are too stupid to recognize the traditional danger signs—jaw pain, chest pain, shoulders or neck pain, numbness in the left arm— a simple electrocardiogram [EKG] or a stress echo test will usually confirm the diagnosis. That is not generally the case in women. Of the estimated 12 million women with some form of heart disease, a quarter of them go undiagnosed because cholesterol plaque does not build into major blockages, but instead spreads evenly throughout the small artery walls, and is almost completely undetectable. When women—and occasionally men—go to their doctors complaining of shortness of breath and fatigue, ischaemia is more often than not misdiagnosed. When doctors use standard angiographic tests to check for blockages, CMS is almost always missed. Standard blood work tests may reveal elevated levels of bad cholesterol and evidence of angina, but not the severeness of the underlying cardiovascular disease. It is the failure to recognize ischaemia that causes the greater proportion of sudden death cardiac events in women.
Unfortunately, most cardiac research is based on white, middle-aged men. Most cadavers used by medical schools are the preserved corpses of white, middle-aged men—even though the medical community over the last few decades have been forced to acknowledge that men and women experience heart disease differently. "More and more," Dr. Frank Smart, MD—a cardiologist and Director of Advanced Heart Failure/Cardiac Transplantation at the Texas Heart Institute—said, "we're finding that men and women experience heart disease very differently. Physicians need to take women's health complaints seriously and understand that not all of the guidelines apply to women whose heart symptoms may appear nonspecific. It's important for women to have a good working relationship with their doctor and be aware of their own risk factors for heart disease."
The study Smart referenced shed light on just how differently women experience heart attacks than men. The study—which examined more than 500 women—found that 95% had developed new and specifically different symptoms up to a month or so before their heart attacks. Topping the list of complaints? Fatigue, restlessness and sleep problems. More than 70% of those interviewed said they experienced no chest discomfort as men do, and had no chest, back, neck, or shoulder pain—and no numbness or pain in the arms. Most of the women dismissed their symptoms as signs of stress related to their lifestyle. Some of those who sought medical attention claimed their doctors either completely misdiagnosed their symptoms, or marginalized them. The symptoms the women in the study group described at the time of their heart attacks were indicative of ischaemia. Fifty-eight percent complained of shortness of breath; 55% were experiencing weakness; 43% complained of extreme fatigue; and 39% complained of having a cold sweat and/or dizziness. Less than half had any chest "discomfort"—but none described the pressure, tightness or ache as pain. Those experiencing such discomfort said it occurred in the back and high chest, just below the clavicle.
Shockingly, 96% of the women in the study group had family histories of heart disease. Sixty-two percent had previously been diagnosed with "heart-related problems" such as high cholesterol or greatly elevated levels of triglycerides. Thirty-three percent of the women in the study group had diabetes.
A study done in 2003 in Alberta, Canada may have revealed the answer to the question of why women are more prone to stealth ischemic heart attacks—and why women who get CMS usually live about 5 years longer than men who are affected by ischaemia. Paul Armstrong, the lead researcher of the University of Alberta study concluded that "[b]iologically, women are less likely than men to develop acute coronary syndrome [ACS] at younger ages due to the presumed protective effect of estrogen."
 The
protective effect of estrogen on heart disease has both a positive and
negative impact—with the negative outweighing the positive. While
estrogen appears to help prevent massive arterial blockage in a large
percentage of women as they reach their mid- to late-thirties and early-forties—up
to the onset of menopause—it does something much worse at that time.
It spreads the plaque evenly throughout the small arteries, coating it
in layers that cause slowly cause ischaemia, clogging the oxygen-starved
arteries until blood flow through the heart is constricted and a heart
attack results. Tragically
for women with small-vessel heart disease, as the natural estrogen levels
diminish with age, women who were protected from developing massive artery
wall blockages in their younger years will suddenly experience the same
type of Acute Coronary Syndrome that affects men of the same age group—only
the women will experience more sudden death heart attacks than their male
counterparts who are not affected by CMS
The
protective effect of estrogen on heart disease has both a positive and
negative impact—with the negative outweighing the positive. While
estrogen appears to help prevent massive arterial blockage in a large
percentage of women as they reach their mid- to late-thirties and early-forties—up
to the onset of menopause—it does something much worse at that time.
It spreads the plaque evenly throughout the small arteries, coating it
in layers that cause slowly cause ischaemia, clogging the oxygen-starved
arteries until blood flow through the heart is constricted and a heart
attack results. Tragically
for women with small-vessel heart disease, as the natural estrogen levels
diminish with age, women who were protected from developing massive artery
wall blockages in their younger years will suddenly experience the same
type of Acute Coronary Syndrome that affects men of the same age group—only
the women will experience more sudden death heart attacks than their male
counterparts who are not affected by CMS
What can a woman do? If you experience ongoing shortness of breath (often without any chest pains or discomfort), and seem always to have flu-like symptoms with nausea, cold sweats and clamminess and you fatigue easily, or you experience general weakness and dizziness and you have unexplained feelings of anxiety, loss of appetite and unspecific discomfort, get to the emergency room. You may be suffering a silent heart attack—particularly if you [a] are overweight, [b] smoke, [c] are diabetic, [d] have high cholesterol, [e] have a family history of heart disease, [f] are postmenopausal, [g] under stress, [h] don't see your doctor regularly and don't care for your own medical needs the way you take care of your husband or other family members. If you smoke, quit now. Women who smoke are up to six times more likely to suffer a heart attack or stroke than nonsmoking women. If you don't see your doctor regularly, start today. Know your numbers. Ask your doctor to check your blood pressure, cholesterol (HDL and LDL), triglycerides and blood glucose. Get to know your health numbers and the range they need to be in to keep you healthy.

Copyright © 2009 Jon Christian Ryter.
All rights reserved.